In our prospective study of 66 patients, 14 patients presented with similar symptoms but failed to respond to cluneal nerve TP injection. These patients responded to computerised tomography-guided nerve root blocks and successfully underwent transforaminal endoscopic lumbar decompression and foraminoplasty at pain provocative segments L3 – S1, with excellent or good outcomes. Overall, 52 patients presented with cluneal nerve TP symptoms, of which seven had paravertebral TPs, four of whom suffered iliac crest TP irritation.
Paravertebral or iliac crest cluneal nerve irritation may arise from spinal malposture, malrotation of the pelvis, or tissue dysfunction following open spinal surgery. The combination of steroid injections and correcting postural dysfunction effectively treated nine of the iliac cluneal cohort and one of the paravertebral cohorts at review, 25 – 67 months later.
Cluneal nerve radiofrequency ablation, was performed in patients with prior symptom duration average of 54.8 (14 – 144) months and symptoms significantly reduced by TP steroid injection. Post-ablation they had a sustained reduction in their visual analogue pain score from 7.3 to 1.1 an average of 38.3 (25 – 66) months later.
This study reflects a cautious learning curve. An early (iliac) case had to be repeated, and another large patient required further ablation due to the multiplicity of nerve leashes. Two additional patients required additional early postoperative palliative steroid injections. There were no cases of numbness, infection, or systemic complications. One patient underwent endoscopic foraminoplasty during this follow-up period for the interval onset of different symptoms arising from an extruding disc protrusion.
In this study, 31/52 patients had their presenting symptoms misconstrued as arising from local facet or sacroiliac joints or spinal sources, resulting in inappropriate “pain management” or spinal surgery.
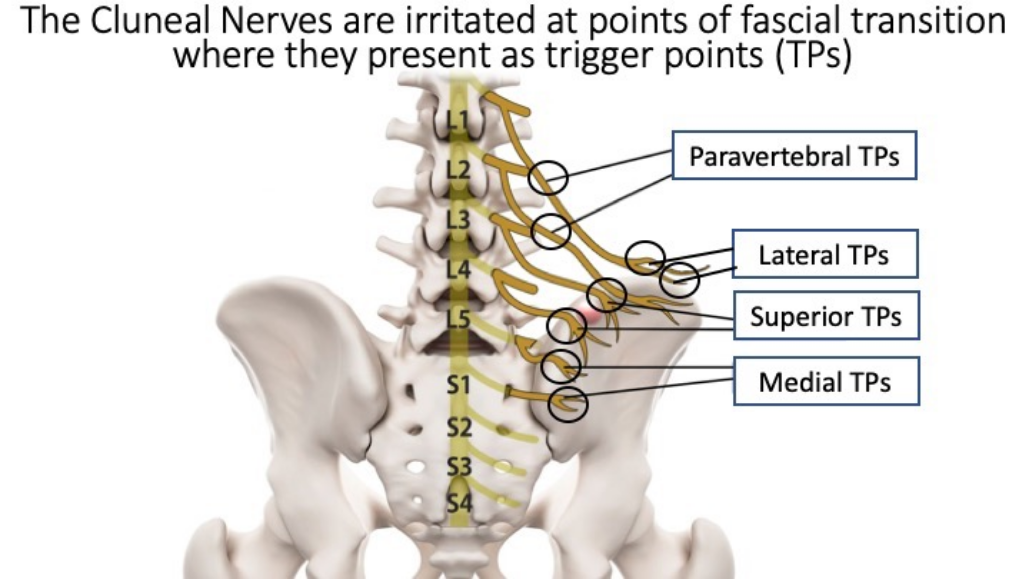
A protocol and anatomical guide to the location of the TPs is included.
Conclusions: Appropriately deployed radiofrequency ablation effectively treats Iliac & paravertebral cluneal TPs irritation – an underdiagnosed entity.
While patients may experience pain on antero-posterior displacement of the midline or facet joint structures, the key feature is the focal tenderness over one or more of the cluneal nerve Trigger Points, the provocation of which replicates some or all of the predominant presenting symptoms.

While core or buttock pain was the predominant feature in these patients, paraesthesia in the limb or even the foot was a frequent symptom in cases of iliac cluneal nerve TP irritation. On occasion, the symptoms were so marked that there was local allodynia in the buttock and paravertebral region, flank, or over the pelvic rim.
Patients with radicular sensory or motor deficits were excluded from this study, although in wider practice this combination can be found, as cluneal nerve irritation often exists in tandem with axial and foraminal spinal pathology. Similarly, paravertebral and iliac TP irritation often occur simultaneously with overlapping symptoms. Paravertebral TPs cause low back pain, which can radiate to the flank, lower abdomen, and even medial groin.
The combination of medial and superior cluneal nerve TP irritation can cause symptoms that radiate over the buttock, posterior thigh, and occasionally through the calf to the sole of the foot mimicking sciatica, but more often produce symptoms over the dorsum or whole foot. These may be paraesthetic, lancinating, causalgic, or occasionally a bursting sensation.
The superior and lateral leashes of the cluneal nerves can produce pain and paraesthesia radiating along the anterolateral thigh. On rarer occasions the symptoms pass into the shin and into the foot, again mimicking sciatica.
The MCN can produce deep medial groin, deep buttock, and sacral–pudendal pain. Indeed, the medial cluneal nerve TP pain is frequently misdiagnosed as pain arising from the sacroiliac joint.
Because cluneal nerve irritation is usually linked to pelvic malposture (anteversion or retroversion) the pain can increase when sitting or getting out of a chair (mimicking the “instability catch”) or can be aggravated by walking or turning in bed. Often, patients have difficulty standing upright.